Blood Sugars and the Menstrual Cycle
Did you know that a woman’s insulin sensitivity changes throughout her monthly cycle? This post will focus on the correlation between monthly fluctuation in hormones and insulin sensitivity so Type 1 diabetic women can better navigate blood sugar management every month. First, let’s walk through the menstrual cycle and its four phases to begin to see why blood sugars may be affected.
Four Phases of the Menstrual Cycle
The total cycle length is around 28 days for many women, but it is possible for cycles to vary in duration. As all diabetics know, everyone is different!
Menstrual: This phase is more commonly called the “period.” During this time, the body sheds the lining of the uterus. As a result, estrogen and progesterone, two critical hormones in the overall cycle, are low during this phase.
Follicular: This phase begins when menstruation starts and ends with the following step, ovulation. During this period, the body produces several follicles in the ovary, each containing an immature egg. However, only one matures.
Ovulation: During ovulation, the mature egg leaves the ovary and begins to make its way toward the uterus through the fallopian tube.
Luteal: The luteal phase is the body’s time to ensure that the lining of the uterus stays thick for a fertilized egg to stick. Hormones that enable this are released by the follicle which housed the mature egg.
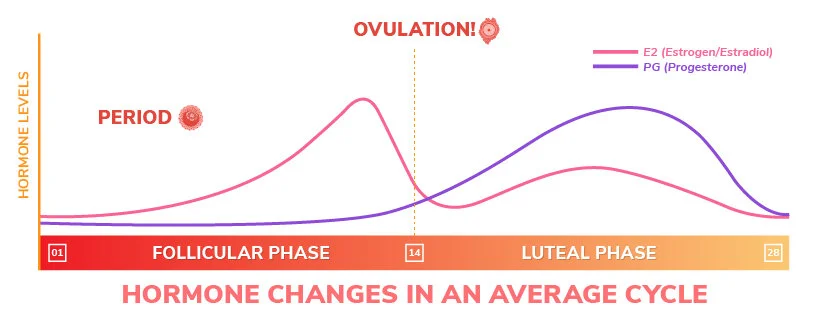
The fluctuation in hormones tends to cause change in blood sugar levels for women at different points in their 28-day cycle. As seen in the chart, estrogen and progesterone are at work in various amounts during the cycle. Progesterone reaches its highest point during the luteal phase, and because higher amounts of progesterone increases insulin resistance, blood sugars are more likely to run higher leading up to the menstrual phase. Both progesterone and estrogen dip down once the menstrual phase begins, increasing insulin sensitivity. Every individual will have different results, even month to month, so it is critical women find their unique trends so they can achieve better control.
Be Prepared: Track Your Period
As a diabetic, the payoff is enormous when you record trends. For example, if you put in the work to track your insulin to carb ratio, then you can hold onto that level for awhile until your physiology feels like switching things up on you, as you know it will!
Of course, you can always keep track using paper and pencil, but there are many apps available to keep track of where you are in the cycle, such as MyFLO or Glow. Over the next couple of cycles, make a note of any irregularities in your blood sugar levels. Stay consistent with your activity and nutrition, so you have fewer variables to consider.
Potential Strategies
First of all, it is a good idea to keep your doctor in the loop. After you gather data, let them know what adjustment you’d like to make!
Basal Changes
Many women discover they need more insulin, especially in the week or so preceding their period. If on a pump, consider creating a separate basal profile or set an increased temporary basal when you experience insulin resistance. If on MDI, you could increase your long-acting insulin.
For safety, you could slowly increase your basal rates until you find the right amount.
Exercise
Go on plenty of walks when you know you’re dealing with resistance because the movement will help lower your stubborn levels.
Be Forgiving
Please realize that your insulin sensitivity may not be affected in the same way every month by your cycle, so you may have to make some tweaks to your basal rates in the moment. Work to nail down more predictable areas, such as nutrition and exercise, so you have less on your mind and can have the energy to adapt. Although it can be overwhelming at first, you will feel more confident knowing how to navigate blood sugars during your cycle once you’ve put in the work to pin down patterns and adjust your basal insulin.
Feel free to share this information with other type 1 diabetic women in your life! Understanding is power when it comes to handling your blood sugar because it is the prerequisite for action.
T1D and recent graduate of the Diabetes In Action program,
Annie Elfelt



![[Endurance Exercise] Nutrition Plans](https://images.squarespace-cdn.com/content/v1/58fdac9e2e69cf0c60bc938f/1704397956588-E0MJLPL5Z998FSBXPREG/20230507_085839.jpg)







6 a.m. hits and my alarm clock goes off for Day 1 of our family vacation in 2014. I had put my spare insulin vial in the hotel fridge the night before along with an apple and yogurt that I wanted to have fresh for breakfast…
I opened the fridge door, and to my horror, my insulin vial had ice crystals frozen over the outside (which rendered it essentially useless).